- Deutsch
- English
Informationen für Therapeuten
Warum Lebensmittel-Allergie-Tests?
Lebensmittelallergien/ -sensitivitäten und Darmgesundheit sind untrennbar miteinander verbunden.
Eine Darm-Mikrobiota im Gleichgewicht und eine intakte Darmbarriere sind Grundlage für die Funktionsfähigkeit des Darms. Nur so kann der Darm die vielfältigen Aufgaben wie Resorbtion, Abwehrleistung, Regulation des Mineralstoff- und Elektrolythaushaltes und Produktion von Enzymen, Hormonen, Botenstoffen und Vitaminen erfüllen.
Die Darmschleimhaut bildet die größte Grenzfläche unseres Körpers zur Außenwelt. Lebensmittelallergien und -sensitivitäten führen auf dieser großen Grenzfläche zu Entzündungen. Dadurch wird die Darmbarriere empfindlich gestört und deren oben beschriebenen Funktionen stark beeinträchtigt. Fortwährende Entzündungen durch Lebensmittelallergien führen zu Leaky Gut. Leaky Gut erhöht die Möglichkeit weiterer Lebensmittelallergien. Ein Teufelskreis! Das Immunsystem gerät aus dem Gleichgewicht, die Immuntoleranz ist beeinträchtigt und es kann zu einem hyperreaktiven Immunsystem kommen. TH1, TH2, TH17 und Treg und damit auch die Bildung von IL2, IL4, IL10 und IL17 geraten aus der Balance. Dies kann zu vielfältigen Symptomen im ganzen Körper führen.
Lebensmittel-Allergie-Tests können helfen diesen Teufelskreis zu durchbrechen. Wenn die inflammatorisch wirkenden Lebensmittel identifiziert und eliminiert werden, beginnt die Darmschleimhaut zu heilen und die Darmbarriere wird wieder hergestellt.
Was wird beim P88 getestet?
Der P88 Lebensmittel-Allergie-Test untersucht vier verschiedene Immunreaktionen auf 88 Lebensmittel:
IgE / IgG4 / IgG / Komplement
Sowohl Lebensmittel-Allergien als auch -Sensitivitäten werden gemessen und ausgewertet.
1. IgE
Immunglobulin E ruft Immunreaktionen des Soforttyps hervor. Unmittelbar bis eine halbe Stunde nach Kontakt mit dem Allergen treten Symptome wie Schwellung, Nesselsucht, Flush oder Atembeschwerden auf. In schweren Fällen führen IgE-Reaktionen zu einem anaphylaktischen Schock.
2. IgG4
Immunglobulin G Subtyp 4 unterscheidet sich grundlegend von Immunglobulin G1, G2 und G3. IgG4 kann die Histamin-Ausschüttung bei einer allergischen Sofortreaktion reduzieren, indem es die Bindung von IgE an den Rezeptor inhibiert. Genau diesen Mechanismus macht man sich bekanntermaßen bei der Hyposensibilisierung zunutze. Hierbei wird nicht etwa IgE reduziert, sondern man erreicht, dass der IgG4 Titer ansteigt. Ist dieser gleich oder höher als IgE ist Immuntoleranz erreicht. Anders als IgG1-3 hat IgG4 nur eine sehr schwache Affinität zu Komplement und Effektorzellen. IgG4 selbst wirkt also kaum entzündlich.
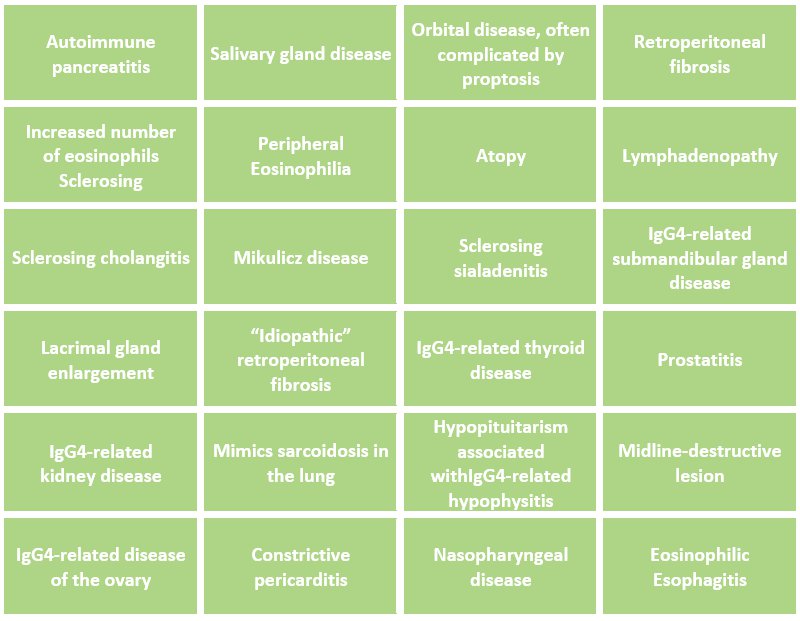
Sehr hohe IgG4 Titer allerdings werden mi Autoimmunerkrankungen in Zusammenhang gebracht. IgG4-RD (IgG4- related diseases) können verschiedene Gewebe betreffen, darunter zum Beispiel Oesophagus, Lymphknoten und Pankreas sowie hormonproduzierende Gewebe wie Schilddrüse, Eierstöcke und Prostata.
Wegen seiner besonderen Eigenschaften ist es sinnvoll IgG4 separat zu messen. (zusätzlich zu IgG gesamt und IgE! Es ergibt sich aus den obigen Erläuterungen, dass die alleinige Bestimmung von IgG4, nicht sinnvoll ist.)
Bei der gemeinsamen Messung von IgG4 und IgE erhält man ein Bild über Immuntoleranz. Lebensmittel bei denen eine Immuntoleranz festgestellt wird müssen dann nicht unnötigerweise aus der Ernährung eliminiert werden.
Bei bereits vorhandenen IgG4-assoziierten Erkrankungen kann sich die Elimination von IgG4-positiven Lebensmitteln günstig auswirken.
IgG4-Assoziierte Erkrankungen (IgG4-RDs):

3. IgG total
Anders als bei IgE treten die Symptome bei IgG-Reaktionen erst 3 bis 72 Stunden nach Kontakt zu Allergenen auf und die betreffenden Lebensmittel können dadurch schwer identifiziert werden. Außerdem unterscheiden sich die Symptome stark. Die Nahrungsmittelsensitivitäten sind subtiler und reichen von Müdigkeit über Kopfschmerzen, Übelkeit, Krampfanfällen, Hyperaktivität, Blähungen, Durchfall, Verstopfung bis hin zu Stimmungsschwankungen. Die Ausprägung der Symptome variiert stark von Person zu Person. IgG–Antikörper haben eine deutlich längere Halbwertszeit als IgE-Antikörper. Die unspezifischen Symptome werden oft jahrelang oder manchmal ein Leben lang nicht mit Lebensmittelsensitivitäten in Zusammenhang gebracht.
Zahlreiche Studien belegen die Verbesserung der Symptome bei Reizdarmsyndrom, ADHS und Rheumatoider Arthritis, wenn IgG-positive Lebensmittel aus der Ernährung über einen gewissen Zeitraum (je nach Höhe des IgG Titers) eliminiert werden.
Mit dem P88-DIY-Lebensmittel-Antigen-Test werden IgG-positive Lebensmittel zuverlässig erkannt.
4. Komplement (C3d)
Komplement, ein Plasma-Protein, ist Teil des angeborenen Immunsystems das normalerweise von Mikroorganismen (z.B. Bakterien, Viren, Hefen, Parasiten) aktiviert wird. Die Komplementaktivierung kann aber auch durch Lebensmittel-Allergene erfolgen. Durch Komplement wird eine IgG-Immunreaktion 1000 bis 10000fach verstärkt. Eine moderate IgG-Immunreaktion auf ein Lebensmittel mit Anwesenheit von Komplement wird also deutlich stärkere Symptome hervorrufen als eine starke IgG-Immunreaktion ohneAnwesenheit von Komplement. Nur wenn man beide Werte kennt, erschließt sich welche Lebensmittel tatsächlich die stärksten Entzündungsreaktionen auslösen.
Komplement teilt sich in verschiedene Fragmente. Eines davon ist C3d, das stabil und gut messbar ist.
Der P88-DIY-Lebensmittel-Antigen-Test erlaubt durch das gleichzeitige Messen von IgG-Gesamt und C3d eine Gewichtung der Lebensmittelsensitivitäten. Nur so kann ermittelt werden welche Lebensmittel tatsächlich die stärksten Entzündungen hervorrufen.
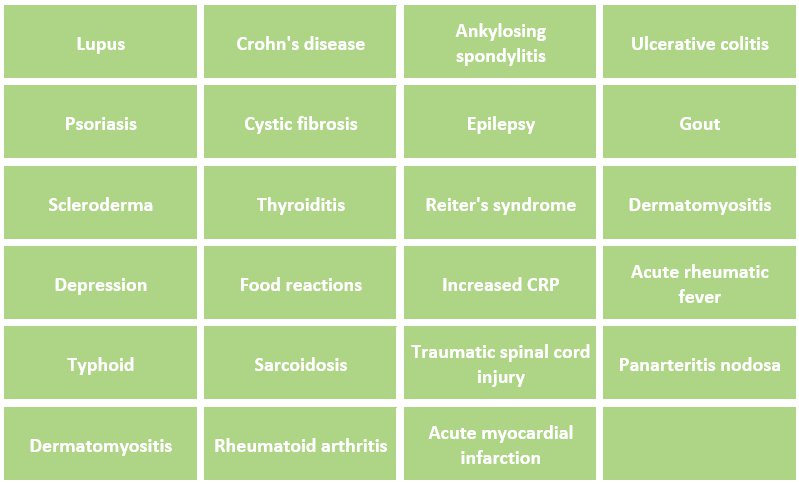
Komplement (C3d) assoziierte Erkrankungen:


P88 IMMUN-INDEX
Nur der Precision Point P88-DIY-Lebensmittel-Antigentest misst mit IgE, IgG4, IgG-Gesamt und Komplement (C3d) gleichzeitig vier verschiedene Immunreaktionen, die bei Lebensmittel-Allergien und -Sensitivitäten relevant sind, in einem einzigen Test.
Jedes im P88 gemessene Nahrungsmittel wird basierend auf den einzelnen Ergebnissen bei den verschiedenen Antikörpertypen und deren Reaktionsniveau mithilfe einer komplexen Berechnung gewichtet. Alle Lebensmittel können dann entsprechend der jeweiligen Gesamt-Reaktivität in absteigender Reihenfolge gelistet werden.
Der Immun-Index ist das Herz des P88-DIY-LM-Antigen-Tests
Mit dem Immun-Index hat man ein innovatives Werkzeug, mit dem gezielt und individuell diejenigen Lebensmittel aus der Ernährung eliminiert werden können, die die stärksten Entzündungsreaktionen verursachen.
Dabei werden nicht wie bei anderen Tests unnötigerweise Lebensmittel eliminiert, bei denen Immuntoleranz vorliegt oder reaktive Lebensmittel übersehen, weil nur auf eine Immunreaktion getestet wird und andere unberücksichtigt bleiben.
Quellenangaben
- Sources: [1] Scand J Gastroenterol. 2014 Jun; 49(6):681-9. Doi: 10.3109/00365521.2014.898326. Epub 2014 Apr 2.
- J Int Med Res. 2012;40(1):204-10. The value of eliminating foods according to food-specific immunoglobulin G antibodies in irritable bowel syndrome with diarrhoea. Guo H, Jiang T, Wang J, Chang Y, Guo H, Zhang W.
- Scand J Gastroenterol. 2005 Jul;40(7):800-7. Food-specific IgG4 antibody-guided exclusion diet improves symptoms and rectal compliance in irritable bowel syndrome. Zar S, Mincher L, Benson MJ, Kumar D.
- Turk J Gastroenterol. 2012 Feb;23(1):19-27. The effects of provocation by foods with raised IgG antibodies and additives on the course of Crohn’s disease: a pilot study. Uzunısmaıl H, Cengız M, Uzun H, Ozbakir F, Goksel S, Demırdağ F, Can G, Balci H.
- Digestion. 2010;81(4):252-64. doi: 10.1159/000264649. Epub 2010 Jan 30. Clinical relevance of IgG antibodies against food antigens in Crohn’s disease: a double-blind cross-over dietintervention study. Bentz S, HausmannM, Piberger H, Kellermeier S, Paul S, Held L, Falk W, Obermeier F, Fried M, Scholmerich J, Rogler G.Division of Gastroenterology and Hepatology, University Hospital Zurich, Zurich, Switzerland.
- Immunobiology. 2012 Nov;217(11):1067-79. The immunoglobulin, IgG Fc receptor and complement triangle in autoimmune diseases. Karsten CM, Kohl J.
- Germany.Int J Rheumatol. 2012;2012:602809. Epub 2012 Aug 26. Pathologies Associated with Serum IgG4 Elevation. Ebbo M, Grados A, Bernit E, Vely F, Boucraut J, Harle JR, Daniel L, Schleinitz N.
- Thirty-four years since the discovery of gastrointestinal melatonin. Bubenik GA.
- Med Hypotheses. 2009 Sep;73(3):438-40. doi: 10.1016/j.mehy.2009.03.037. Epub 2009 Apr 29. The gluten syndrome: a neurological disease. Ford RP.
- Pediatrics. 2004 Jun;113(6):1672-6. Range of neurologic disorders in patients with celiac disease. Zelnik N, Pacht A, Obeid R, Lerner A.adults.
- Med Hypotheses. 2008;70(1):73-80. Epub 2007 Jun 14. The minicolumnopathy of autism: A link between migraine and gastrointestinal symptoms. Casanova MF.
- J Altern Complement Med. 1999 Dec;5(6):575-86. The abdominal brain and enteric nervous system. McMillin DL, Richards DG, Mein EA, Nelson CD.
- ClinObstet Gynecol. 2013 Apr 4. [Epub ahead of print] Headaches During Pregnancy. Digre KB.
- J Immunol. 2011 Sep 1;187(5):2646-55. Epub 2011 Aug 1. A strain of Lactobacillus casei inhibits the effector phase of immune inflammation. Schiffer C, Lalanne AI, Cassard L, Mancardi DA, Malbec O, Bruhns P, Dif F, DaeronM.
- Acta Med Indones. 2010 Oct;42(4):236-40. Recurrent aphthous stomatitis caused by food allergy. Wardhana, Datau EA.
- Scand J Gastroenterol. 2012 Sep;47(8-9):914-9. doi: 10.3109/00365521.2012.690045. Epub 2012 May 18. Functional bowel symptoms, fibromyalgia, and fatigue: a food-induced triad? Berstad A, Undseth R, Lind R, Valeur J.
- Ann Allergy. 1991 Feb;66(2):181-4. Intestinal permeability in patients with chronic urticaria-angioedema with and without arthralgia. Paganelli R, Fagiolo U, Cancian M, Scala E.
- Clin Infect Dis. 2013 Mar 26. IgG Anticardiolipin Antibodies and Progression to Q Fever Endocarditis. Million M, Walter G, Bardin N, Camoin L, Giorgi R, Bongrand P, Gouriet F, Casalta JP, Thuny F, Habib G, Raoult D.Unite de Recherche sur les Maladies Infectieuses et Tropicales Emergentes, Faculte de Medecine, CNRS UMR 7278, IRD 198, Aix-Marseille Universite, 27 Bd Jean Moulin, 13005 Marseille, France.
- Marijn van der NeutKolfschoten, et al Anti-Inflammatory Activity of Human IgG4 Antibodies by Dynamic Fab Arm Exchange. SCIENCE VOL 317 14 SEPTEMBER 2007 pgs1554-1555.
- Volpi, Nicola and Maccari, Francesca(2009) ‘Serum IgG Responses to Food Antigens in the Italian Population Evaluated by Highly Sensitive and Specific ELISA Test’, Journal of Immunoassay and Immunochemistry, 30: 51 — 69.
- Kemeny DM, et al Sub-class of IgG in allergic disease. I. IgG sub-class antibodies in immediate and non-immediate food allergy. Clin Allergy. 1986 Nov; 16(6):571-81.
- Stapel SO, Testing for IgG4 against foods is not recommended as a diagnostic tool: EAACI Task Force Report.Allergy. 2008 Jul;63(7):793-6. Epub 2008 May 16.
- Statement of the AAAAI Work Group Report: Current approach to the diagnosis and management of adverse reactions to foods [web page]. October 2003. , 2013
- Dixon H. Treatment of delayed food allergy basd on specific immunoglobulin G RAST testing relief. Otoloryngol Head Neck Surg. 2000; 1234:48-54
- NagisaSugaya N, Nomura S. Relationship between congnitive appraisals of symptoms and negative mood for subtypes of irritable bowel syndrome. BioPsychoSocial Medicine 2008; 2:9-14.
- Atkinson W et al. Food elimination based on IgG antibodies in irritable bowel syndrome: a randomized controlled trial. Gut 2004; 53:1459-1464.
- Drsko J, Bischoff B, Hall M, McCallum R. Treating irritable bowel syndrome with a food elimination diet followed by food challenge and probiotics. J Am CollNutr. 2006; 25: 514-522.
- Bentz S. et al. Clinical relevance of IgG antibodies against food antigens in Crohn’s disease: a double-blind cross-over diet Saccharomycesmannan antibodies (ASCA) of Crohn’s patients cross react with mannan from other yeast strains, and murine ASCA IgM can be experimentally induced with Candida albicans. Inflamm Bowel Dis. 2007; 13: 1339-1346.
- Hadjivssilou M, Grunewald RA, Davies-Jones GAB. Gluten sensitivity as a neurological illness. Nerol/Neurosurg Psychiatry. 2002; 72: 560-563.
- Vladimir T et al. Higher plasma concentration of food-specific antibodies in persons with autistic disorder in comparison to their siblings. Focus Autism other Dev Disabl. 2008; 23: 176-185.
- Severance EG et al. Subunit and whole molecule specificity of the anti-bovine case in immune response in recent onset psychosis and schizophrenia. Schizophr Res. 2010; 118: 240-247.
- Huber A et al. Diet restriction in migraine, based on IgG against foods: a clinical double-blind, randomized, cross-over trial. Int Arch Allergy Immunol. 1998; 115: 67-72.
Info for health care providers
Why food allergy and sensitivity testing?
Food allergies/sensitivities and gut health are inseparable.
An intestinal microbiota in balance and an intact intestinal barrier are fundamental for a well-functioning intestine.
Only then, the intestine fulfils the various tasks such as absorption, defence, regulation of the mineral and electrolyte balance and production of enzymes, hormones, messenger substances and vitamins.
The intestinal mucosa forms the largest interface between our body and the outside world. Food allergies and sensitivities lead to inflammation at this large interface. As a result, the intestinal barrier is severely disturbed and its functions described above are severely impaired. Ongoing inflammation caused by food allergies leads to leaky gut. Leaky gut increases the possibility of further food allergies. A vicious circle! The immune system becomes unbalanced, immune tolerance is impaired and can lead to a hyperreactive immune system. TH1, TH2, TH17 and Treg and thus also the formation of IL2, IL4, IL10 and IL17 get out of balance. This can lead to a variety of symptoms throughout the entire body.
Food allergy testing can help breaking this vicious cycle. When we can identify and eliminate the foods that provoke inflammatory reactions, the intestinal mucosa begins to heal, and the intestinal barrier will be restored.
What are we testing for?
The P88 Food Allergy Test examines four different immune responses to 88 different foods. Both, food allergies and sensitivities are measured and evaluated.
1. IgE
Immunoglobulin E provokes immune reactions of the immediate type. Immediately and up to half an hour after contact with the allergen, symptoms such as swelling, hives, flushing or difficulty breathing occur. In severe cases, IgE reactions lead to anaphylactic shock.
2. IgG4
Immunoglobulin G subtype 4 is fundamentally different from immunoglobulin G1, G2 and G3. IgG4 can reduce histamine secretion in an immediate allergic reaction by inhibiting the binding of IgE to the receptor. It is precisely this mechanism that is used in hypo sensitization. The hypo sensitization therapy does not reduce IgE but increases the IgG4 titer. A IgG4 titer equal or higher than IgE leads to immune tolerance. Unlike IgG1-3, IgG4 has only a very weak affinity to complement and effector cells. So, IgG4 itself is much less inflammatory than IgG1-3. Because of its special characteristics, it makes sense to measure IgG4 separately. (In addition to IgG total and IgE! – As explained above the solely determination of IgG4 is not sufficient.)
Though IgG4 does not always result in a negative prognosis, with certain conditions, higher levels of IgG4 can be harmful. IgG4-RD (IgG4-related diseases) can affect various tissues, including the esophagus, lymph nodes, and pancreas, as well as hormone-producing tissues such as the thyroid, ovaries and prostate.
IgG4-Related Diseases (IgG4-RDs)
3. IgG total
Unlike IgE, the symptoms of IgG reactions do not appear until 3 to 72 hours after contact with allergens, making it difficult to identify the foods in question. In addition, the symptoms differ greatly. Food sensitivities are more subtle and range from fatigue to headaches, nausea, seizures, hyperactivity, bloating, diarrhea, constipation, and mood swings. The severity of the symptoms varies from person to person. IgG antibodies have a significantly longer half-life than IgE antibodies. The non-specific symptoms are often not associated with food sensitivities for years or sometimes a lifetime.
Numerous studies show the improvement of symptoms such as irritable bowel syndrome, ADHD, and rheumatoid arthritis when IgG-positive foods are eliminated from the diet over a period of time (depending on the level of the IgG titer).
With the P88 DIY food antigen test, IgG-positive foods are reliably detected.
4. Complement (C3d)
Complement, a plasma protein, is part of the innate immune system. Normally it is activated by microorganisms (such as bacteria, viruses, yeasts, parasites). However, complement activation can also be caused by food allergens. Through complement, an IgG immune reaction can be increased 1000 to 10000 times. A moderate IgG immune reaction to a food with the presence of complement will therefore produce significantly stronger symptoms than a strong IgG immune reaction without the presence of complement. Only if you know both values, it is clear which foods trigger the strongest inflammatory response.
Complement is degraded into different fragments. One of them is C3d, which is stable and easily measurable. The P88 DAT is the only test that additional to IgG also measures Complement C3d. Tests that only measure IgG may miss the reactions to foods that are most clinically relevant.
Conditions associated with Complement (C3d):
P88 IMMUNE INDEX
Common Allergy or Sensitivity testing only looks at one way the body reacts to foods. However, there are multiple ways the immune system responds to antigens, so unless you measure multiple reactions or antibodies, you will miss foods a patient reacts to.
The P88 DAT looks at four immune reactions, including IgE (Allergies) IgG (Sensitivities) as well as IgG4, and C3d, all specific to eighty-eight foods. Then, based on each antibody type and their level of reaction, a calculation is done to give the patient their overall reactivity to each food. The P88 DAT Report shows the level of reaction based on each antibody, but then also gives a cumulative score which we named P88 Immune-Index.
The P88 IMMUNE Index is an innovative approach and tool:
The P88 Immune Index gives the practitioner a sliding scale to remove as many or as few reactive foods as needed from the diet based on their relative level of reaction. In addition, rather than basing results on just one type of immune reaction, you are basing it on all types combined.
An allergy is mediated by IgE antibodies and creates an immediate reaction. A sensitivity is created by IgG antibodies and create a delayed response. While these general traits hold true, there are also times when IgG can amplify IgE reactions, and also some examples of if there is a remarkably high level of IgG, it can have more of an immediate reaction too. They create independent reactions but can also influence each other. IgG is most typically a delayed reaction, but if high enough titers are present, it too can react within a few hours. The interplay between parts of the immune system demonstrates why it is best to look at multiple antibodies together.
Complement plays a role in how inflammatory an IgG antibody is. Complement binds to IgG and creates a synergistic effect in terms of increasing inflammation. The combination of complement and IgG together can increase inflammation 1000 to 10,000-fold.
IgG4 is indicative of immune tolerance. IgG4 can reduce histamine secretion in an immediate allergic reaction by inhibiting the binding of IgE to the receptor. By measuring both IgE and IgG4 you can determine the severity of your patient’s reaction to certain foods. However, there are a handful of conditions that increase IgG4 reactions. When a patient has IgG4-RDs it may be helpful to remove foods that are IgG4 positive.
IgE and IgG should be measured together because they each independently play a role in symptoms to foods. You can either have an allergy/IgE response, or a sensitivity IgG response and both are independent of the other and create inflammation in the body.
Only testing IgG, is a bit like knowing total cholesterol, but not knowing how much HDL/good or LDL/bad cholesterol you have. The reason for this is that different IgG antibodies do different things depending on their subtype. IgG4 decreases IgE or allergic reactions. IgGI-III increase inflammation 3-72 hours after exposure.
Also, different subtypes are increased in certain pathologies. For example, while IgG4 is generally good, there are a handful of pathologies where it is of concern, such as auto-immune hypothyroidism and eosinophilic esophagitis.
IgG4 is by and large good, as it blunts an IgE response and reduces anaphylactic shock. In fact, desensitization injections and drops work by this mechanism of increasing Ig4 to induce tolerance. However, there are a handful of conditions that increase IgG4 reactions, and if the patient has one of these conditions it may be helpful to remove foods that are provoking an IgG4 reaction.
Gluten is in whole wheat; however, wheat has other proteins that you could react to. It is possible for someone to come back positive to wheat and not gluten, and that would mean you are reactive to other proteins in the wheat instead of the gluten.
If your patient comes back positive to gluten, but not to wheat, it is because the other proteins in wheat can obscure a bit of the binding to gluten, so it is also isolated, and run separately. We do this is to catch smaller gluten reactions that did not show up because of other proteins obscuring reactions and because you will capture lower-level reactions that are only seen when gluten is isolated. Because it is such an antigenic molecule, it is important to see if even minimal amounts will trigger reactivity.
Reactions to gluten could be because of allergies or sensitivities, but there are also a number of other reasons you can feel bad from gluten outside of sensitivities. For example, gluten more than other grains decreases the tryptophan to serotonin ratio, making production of this neurotransmitter more difficult. Also, gluten can often be contaminated with bromides that decreases other important nutrients like Iodine which compromises thyroid function.
Gluten can often be moldy, as commercial grains are measured for ppm of aflatoxin and are gener- ally positive for this contaminate.
Of course, nobody would sit in front of a bowl of moldy food and eat it. But allergy or sensitivity to mold worsens chronic conditions. After detecting positive immune reactions to mold potentially moldy foods should be avoided. Mold in the environment also must be taken into consideration.
MOLDS TESTED INCLUDE: Asper-gillus (A. oryzae, A. niger, A repent, A. terries).
Key foods to avoid for elevated mold reaction are moldy cheeses, peanuts, melons, and sake. Vinegar & Vinegar containing food (food (mayonnaise, salad dressings, catsup, chili sauce, pickled foods, relishes, green olives, mustard ), Alcohol, Soured Breads, Sauerkraut, Cider & Root beer, pick- led & smoked meats. All dried fruits, Canned tomatoes (unless homemade), & all canned juice.
Only freshly opened canned foods & freshly prepared foods should be consumed. Meat or fish should not be more than 24 hours old. Avoid food from leftovers and avoid Hamburgers if not made from freshly ground meat.
For patients with severe reactions and active symptoms, a more restrictive mold diet may be needed. Consider using Konjac Fiber, which binds to mold aflatoxin.
The P88-DIY meassures the immune response to mold. It can not answer the question of the mold exposure. Besides moldy foods also the living environment and working place has to be taken into considaration.
Cross-reactivity occurs when the protein structure of one substance is similar to another. Our body's immune system may react to the similar structure as it would to the true allergen. Cross-reactivity can occur to other foods as well as the envirement such as airborne antigens (pollen, mite feces...) or contact antigens (latex). This way it is possible there is a positive immune reaction to a food that is never consumed.
When a food that is never consumed shows up positive in the test we first have to rule out hidden sources in the diet. The next most likely explanation is that there is cross-reactivity. Cross-reactivity does not only happen from foods in the same food family, but also from things in the environment to foods as well. For example, someone who is reactive to beef, but is vegetarian, may have been bitten by a tick as there is cross-reactivity between beef immunoglobulins and tick antibodies. If one is sensitive to latex, you may also be sensitive to bananas as well, because they are in the same family. Cross-reactivity may explain many unusual reactions, and a complete list of cross-reactivity between foods and the environment, and food families can be found in our Physicians Guide to the P88 DAT.
IgG reactions are both the cause and the result of gut-based permeability. One way we develop IgG reactions is when the gut becomes more compromised or permeable. This allows for larger molecules than normal to “leak” through the gut. These larger molecules look antigenic to the immune system. T cells become sensitized and begin to make an immune response or produce antibodies. However, this is not the only way one can become sensitive to foods. Improper immune queuing in the GI tract, specifically in cells called the Peyer’s patches, can also cause this too.
Once an IgG reaction begins, it increases production of histamine and inflammation. This inflammation continues to damage the gut, thereby contributing to permeability. The best way to reduce gut-based inflammation, is to remove offending foods and work on healing the gut.
Reactions to gluten could be because of allergies or sensitivities, but there are also a number of other reasons you can feel bad from gluten outside of sensitivities. For example, gluten more than other grains decreases the tryptophan to serotonin ratio, making production of this neurotransmitter more difficult. Also, gluten can often be contaminated with bromides that decreases other important nutrients like Iodine which compromises thyroid function.
Gluten can often be moldy, as commercial grains are measured for ppm of aflatoxin and are generally positive for this contaminate.
Food sensitivities can be related to weight gain in that they will create more inflammation in the body. Inflammation will cause an increase in the hormone leptin, which in turn tells adipose tissue to store more fat. Inflammatory foods create and irritation that leads to weight gain.
Foods causing an immune reaction can cause symptoms itself, but also decrease thyroid activity. IgG4 reactions to foods have been shown to specifically damage the thyroid tissue. Complement reactions also damage thyroid tissue. This is the only food test that looks at the exact components that are most damaging to the thyroid. Immune reactions to foods create inflammation. This inflammation causes the body to be less able to convert T4 into T3. Ongoing exposure to foods which cause immune reactions, can increase antibody production, causing the body to attack thyroid tissue. Eliminating foods, a person is sensitive to is a great first step to increasing thyroid function naturally.
Yes! While the beginning of the reaction to foods starts in the gut, it does not have to necessarily create gut pain, or be contained in the GI tract. The inflammatory process that starts in the gut can spread and even be more symptomatic in places outside of the gut. Many conditions such as head- aches, pain and even depression have a gut-based cause but manifest in other areas of the body.
Every lab is required to develop their own reference ranges. For this reason, you should not expect ranges to be the same from lab to lab.
At Precision, we look at the values over the hundreds of thousands of specimens we have run, and then looked at distributions. In general, the top 5% is determined high (>95%), and then the next 20% is moderate (>75%-95%), and then the next 65% is low. The remaining 10% are considered as no reaction.
However, when there is epidemiologic evidence that the population in general has more difficulty with a food, such as dairy, casein, wheat, gluten, egg, shellfish and tree-nuts we will consider %-reactivity in populations in general, and consider research and data, alongside our distributions to create a range. High range in foods with a greater pevalence of reactivity in the general population is defined as the top 10% (>90%), moderate range as the next 40% (>50%-90%), and low range as the next 40% (>10%-50%). Again, the remaining 10% are considered as no reaction.
For 399€ the test measures four immune reactions in one test with an extensiv report including an alphabetically summary, two different diet suggestions and the Immune Index.
References
- Sources: [1] Scand J Gastroenterol. 2014 Jun; 49(6):681-9. Doi: 10.3109/00365521.2014.898326. Epub 2014 Apr 2.
- J Int Med Res. 2012;40(1):204-10. The value of eliminating foods according to food-specific immunoglobulin G antibodies in irritable bowel syndrome with diarrhoea. Guo H, Jiang T, Wang J, Chang Y, Guo H, Zhang W.
- Scand J Gastroenterol. 2005 Jul;40(7):800-7. Food-specific IgG4 antibody-guided exclusion diet improves symptoms and rectal compliance in irritable bowel syndrome. Zar S, Mincher L, Benson MJ, Kumar D.
- Turk J Gastroenterol. 2012 Feb;23(1):19-27. The effects of provocation by foods with raised IgG antibodies and additives on the course of Crohn’s disease: a pilot study. Uzunısmaıl H, Cengız M, Uzun H, Ozbakir F, Goksel S, Demırdağ F, Can G, Balci H.
- Digestion. 2010;81(4):252-64. doi: 10.1159/000264649. Epub 2010 Jan 30. Clinical relevance of IgG antibodies against food antigens in Crohn’s disease: a double-blind cross-over dietintervention study. Bentz S, HausmannM, Piberger H, Kellermeier S, Paul S, Held L, Falk W, Obermeier F, Fried M, Scholmerich J, Rogler G.Division of Gastroenterology and Hepatology, University Hospital Zurich, Zurich, Switzerland.
- Immunobiology. 2012 Nov;217(11):1067-79. The immunoglobulin, IgG Fc receptor and complement triangle in autoimmune diseases. Karsten CM, Kohl J.
- Germany.Int J Rheumatol. 2012;2012:602809. Epub 2012 Aug 26. Pathologies Associated with Serum IgG4 Elevation. Ebbo M, Grados A, Bernit E, Vely F, Boucraut J, Harle JR, Daniel L, Schleinitz N.
- Thirty-four years since the discovery of gastrointestinal melatonin. Bubenik GA.
- Med Hypotheses. 2009 Sep;73(3):438-40. doi: 10.1016/j.mehy.2009.03.037. Epub 2009 Apr 29. The gluten syndrome: a neurological disease. Ford RP.
- Pediatrics. 2004 Jun;113(6):1672-6. Range of neurologic disorders in patients with celiac disease. Zelnik N, Pacht A, Obeid R, Lerner A.adults.
- Med Hypotheses. 2008;70(1):73-80. Epub 2007 Jun 14. The minicolumnopathy of autism: A link between migraine and gastrointestinal symptoms. Casanova MF.
- J Altern Complement Med. 1999 Dec;5(6):575-86. The abdominal brain and enteric nervous system. McMillin DL, Richards DG, Mein EA, Nelson CD.
- ClinObstet Gynecol. 2013 Apr 4. [Epub ahead of print] Headaches During Pregnancy. Digre KB.
- J Immunol. 2011 Sep 1;187(5):2646-55. Epub 2011 Aug 1. A strain of Lactobacillus casei inhibits the effector phase of immune inflammation. Schiffer C, Lalanne AI, Cassard L, Mancardi DA, Malbec O, Bruhns P, Dif F, DaeronM.
- Acta Med Indones. 2010 Oct;42(4):236-40. Recurrent aphthous stomatitis caused by food allergy. Wardhana, Datau EA.
- Scand J Gastroenterol. 2012 Sep;47(8-9):914-9. doi: 10.3109/00365521.2012.690045. Epub 2012 May 18. Functional bowel symptoms, fibromyalgia, and fatigue: a food-induced triad? Berstad A, Undseth R, Lind R, Valeur J.
- Ann Allergy. 1991 Feb;66(2):181-4. Intestinal permeability in patients with chronic urticaria-angioedema with and without arthralgia. Paganelli R, Fagiolo U, Cancian M, Scala E.
- Clin Infect Dis. 2013 Mar 26. IgG Anticardiolipin Antibodies and Progression to Q Fever Endocarditis. Million M, Walter G, Bardin N, Camoin L, Giorgi R, Bongrand P, Gouriet F, Casalta JP, Thuny F, Habib G, Raoult D.Unite de Recherche sur les Maladies Infectieuses et Tropicales Emergentes, Faculte de Medecine, CNRS UMR 7278, IRD 198, Aix-Marseille Universite, 27 Bd Jean Moulin, 13005 Marseille, France.
- Marijn van der NeutKolfschoten, et al Anti-Inflammatory Activity of Human IgG4 Antibodies by Dynamic Fab Arm Exchange. SCIENCE VOL 317 14 SEPTEMBER 2007 pgs1554-1555.
- Volpi, Nicola and Maccari, Francesca(2009) ‘Serum IgG Responses to Food Antigens in the Italian Population Evaluated by Highly Sensitive and Specific ELISA Test’, Journal of Immunoassay and Immunochemistry, 30: 51 — 69.
- Kemeny DM, et al Sub-class of IgG in allergic disease. I. IgG sub-class antibodies in immediate and non-immediate food allergy. Clin Allergy. 1986 Nov; 16(6):571-81.
- Stapel SO, Testing for IgG4 against foods is not recommended as a diagnostic tool: EAACI Task Force Report.Allergy. 2008 Jul;63(7):793-6. Epub 2008 May 16.
- Statement of the AAAAI Work Group Report: Current approach to the diagnosis and management of adverse reactions to foods [web page]. October 2003. , 2013
- Dixon H. Treatment of delayed food allergy basd on specific immunoglobulin G RAST testing relief. Otoloryngol Head Neck Surg. 2000; 1234:48-54
- NagisaSugaya N, Nomura S. Relationship between congnitive appraisals of symptoms and negative mood for subtypes of irritable bowel syndrome. BioPsychoSocial Medicine 2008; 2:9-14.
- Atkinson W et al. Food elimination based on IgG antibodies in irritable bowel syndrome: a randomized controlled trial. Gut 2004; 53:1459-1464.
- Drsko J, Bischoff B, Hall M, McCallum R. Treating irritable bowel syndrome with a food elimination diet followed by food challenge and probiotics. J Am CollNutr. 2006; 25: 514-522.
- Bentz S. et al. Clinical relevance of IgG antibodies against food antigens in Crohn’s disease: a double-blind cross-over diet Saccharomycesmannan antibodies (ASCA) of Crohn’s patients cross react with mannan from other yeast strains, and murine ASCA IgM can be experimentally induced with Candida albicans. Inflamm Bowel Dis. 2007; 13: 1339-1346.
- Hadjivssilou M, Grunewald RA, Davies-Jones GAB. Gluten sensitivity as a neurological illness. Nerol/Neurosurg Psychiatry. 2002; 72: 560-563.
- Vladimir T et al. Higher plasma concentration of food-specific antibodies in persons with autistic disorder in comparison to their siblings. Focus Autism other Dev Disabl. 2008; 23: 176-185.
- Severance EG et al. Subunit and whole molecule specificity of the anti-bovine case in immune response in recent onset psychosis and schizophrenia. Schizophr Res. 2010; 118: 240-247.
- Huber A et al. Diet restriction in migraine, based on IgG against foods: a clinical double-blind, randomized, cross-over trial. Int Arch Allergy Immunol. 1998; 115: 67-72.

